Hypertension, commonly known as high blood pressure, is a significant public health issue that affects millions of individuals globally. It is often categorized into different types based on various factors such as time of occurrence, response to treatment, and underlying mechanisms. One important classification is based on the variability of blood pressure throughout the day, particularly focusing on the concepts of “dipper” and “non-dipper” hypertension. This article aims to provide an in-depth understanding of these two types of hypertension, exploring their definitions, implications, diagnostic criteria, and management strategies.
What is Dipper Hypertension?
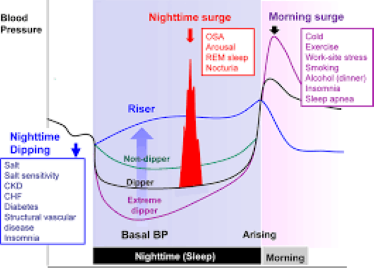
Dipper hypertension refers to a pattern of blood pressure variation where there is a significant decrease in blood pressure during the nighttime compared to daytime levels. This reduction is typically around 10-20% of the daytime blood pressure and is considered a normal physiological response. The term “dipper” derives from the observation that these individuals’ blood pressure dips or decreases during sleep, akin to the dipping motion.
Characteristics of Dipper Hypertension
- Circadian Rhythm: Dipper hypertension follows a natural circadian rhythm where blood pressure decreases at night. This phenomenon is believed to be associated with a variety of physiological processes, including hormonal changes, reduced sympathetic nervous system activity, and improved vascular relaxation.
- Health Implications: Individuals with dipper hypertension are generally considered to have a lower risk of cardiovascular complications compared to those with non-dipper hypertension. The nocturnal dip is associated with a reduced risk of developing end-organ damage and cardiovascular events.
- Diagnostic Criteria: The diagnosis of dipper hypertension is typically made using ambulatory blood pressure monitoring (ABPM). ABPM involves wearing a portable device that measures blood pressure at regular intervals over a 24-hour period. A drop of 10-20% in nighttime blood pressure relative to daytime levels is used to classify an individual as a dipper.
What is Non-Dipper Hypertension?
Non-dipper hypertension refers to a pattern where the expected nighttime drop in blood pressure is either absent or minimal. This means that individuals with non-dipper hypertension have elevated blood pressure throughout the 24-hour period, including during sleep.
Characteristics of Non-Dipper Hypertension
- Lack of Nocturnal Dip: Unlike dippers, individuals with non-dipper hypertension do not experience a significant reduction in blood pressure during the night. In some cases, blood pressure may even rise during sleep.
- Health Implications: Non-dipper hypertension is associated with a higher risk of cardiovascular complications, such as stroke, myocardial infarction, and renal damage. The lack of a nocturnal dip is thought to contribute to sustained stress on the cardiovascular system and increased risk of end-organ damage.
- Diagnostic Criteria: Similar to dipper hypertension, non-dipper hypertension is diagnosed through ABPM. The absence of a significant drop in nighttime blood pressure, typically less than 10% of daytime levels, characterizes non-dipper hypertension.
Factors Influencing Dipper and Non-Dipper Patterns
Several factors can influence whether an individual is a dipper or non-dipper. These include:
- Age: The nocturnal dip in blood pressure tends to become less pronounced with age. Older individuals are more likely to exhibit non-dipper patterns.
- Medications: Certain medications can affect blood pressure patterns. For example, antihypertensive medications may impact the degree of nocturnal dipping.
- Sleep Disorders: Conditions such as obstructive sleep apnea can influence blood pressure patterns, potentially leading to a non-dipper pattern.
- Lifestyle Factors: Factors such as physical activity, dietary habits, and alcohol consumption can impact blood pressure regulation and may influence dipping patterns.
- Underlying Health Conditions: Chronic conditions such as diabetes, chronic kidney disease, and cardiovascular diseases can affect blood pressure variability and contribute to non-dipper patterns.
Diagnostic Approaches
Diagnosing dipper and non-dipper’s hypertension typically involves the use of ambulatory blood pressure monitoring (ABPM). ABPM is considered the gold standard for assessing blood pressure variability and providing a comprehensive overview of blood pressure patterns throughout the day and night.
Ambulatory Blood Pressure Monitoring (ABPM)
- Procedure: ABPM involves the patient wearing a portable blood pressure monitor that takes measurements at regular intervals, usually every 15-30 minutes, over a 24-hour period. The device is worn on the arm and records blood pressure readings while the patient goes about their daily activities.
- Data Analysis: The collected data is analyzed to determine the average daytime and nighttime blood pressure readings. The percentage of blood pressure reduction during the night is used to classify the individual.
- Advantages: ABPM provides a detailed and accurate assessment of blood pressure patterns, offering insights into variations that may not be captured during a single office visit. It helps in identifying individuals at higher risk of cardiovascular complications.
Implications for Management
The management of dipper and non-dipper’s hypertension involves tailored approaches based on the individual’s blood pressure patterns and associated risk factors. Effective management strategies can help mitigate the risk of cardiovascular events and improve overall health outcomes.
Management of Dipper Hypertension
- Lifestyle Modifications: For individuals with dipper hypertension, lifestyle modifications such as maintaining a healthy diet, regular physical activity, and weight management are recommended to support overall cardiovascular health.
- Medication Adherence: Adherence to prescribed antihypertensive medications is crucial for managing blood pressure levels effectively and reducing the risk of complications.
- Regular Monitoring: Regular follow-up with healthcare providers and periodic ABPM assessments are important for monitoring blood pressure patterns and adjusting treatment as needed.
Management of Non-Dipper Hypertension
Intensive Monitoring: Individuals with non-dipper’s hypertension may require more intensive monitoring and management to address the elevated risk of cardiovascular complications. This may involve more frequent ABPM assessments and adjustments to treatment plans.
- Medication Adjustments: Medication regimens may need to be adjusted to address non-dipper’s patterns and ensure effective blood pressure control throughout the 24-hour period. This may include the use of long-acting antihypertensive agents.
- Addressing Underlying Conditions: Identifying and managing underlying conditions such as sleep apnea, diabetes, or chronic kidney disease is crucial for improving blood pressure patterns and reducing cardiovascular risk.
Future Directions and Research
Ongoing research is focused on further understanding the mechanisms underlying dipper and non-dipper’s hypertension, as well as developing targeted interventions to improve outcomes. Some areas of interest include:
- Biomarkers and Genetic Factors: Identifying biomarkers and genetic factors associated with dipper and non-dipper’s hypertension could lead to more personalized approaches to diagnosis and treatment.
- Innovative Monitoring Technologies: Advances in wearable technology and remote monitoring systems may enhance the ability to assess blood pressure patterns more accurately and provide real-time feedback to patients and healthcare providers.
- Interventional Studies: Clinical trials investigating novel interventions and treatment strategies for managing non-dipper’s hypertension could provide new insights and improve outcomes for individuals with this condition.
Conclusion
Dipper and non-dipper hypertension represent distinct patterns of blood pressure variation with important implications for cardiovascular health. Understanding these patterns, their underlying mechanisms, and their impact on health outcomes is essential for effective diagnosis and management. By employing comprehensive diagnostic approaches and tailored management strategies, healthcare providers can improve patient outcomes and reduce the risk of cardiovascular complications associated with hypertension. Continued research and advancements in technology hold promise for further enhancing our understanding and treatment of these hypertension patterns, ultimately leading to better health outcomes for individuals affected by high blood pressure.